Many women find out they have polycystic ovary syndrome (PCOS) when they start trying to conceive. The condition typically affects women in their reproductive years, but it can also occur early in puberty and in menopause.
This article explains the symptoms and possible causes of polycystic ovary syndrome and recommends solutions for symptom management.

What Is Polycystic Ovary Syndrome (PCOS)?
Polycystic ovary syndrome is a complex hormonal disorder with gynecological manifestations typically present during the reproductive period. It is characterized by hormonal imbalances, enlarged ovaries carrying fluid-filled follicles instead of mature eggs, and irregular or absent menstrual cycles.
PCOS is closely related to other medical conditions that cause or stem from PCOS, including inflammation, insulin resistance, type 2 diabetes, and obesity.
Types of PCOS
Medical professionals use two standard classifications to distinguish between PCOS types: by phenotype and by an underlying cause.
Types of PCOS by Phenotype (Rotterdam Criteria)
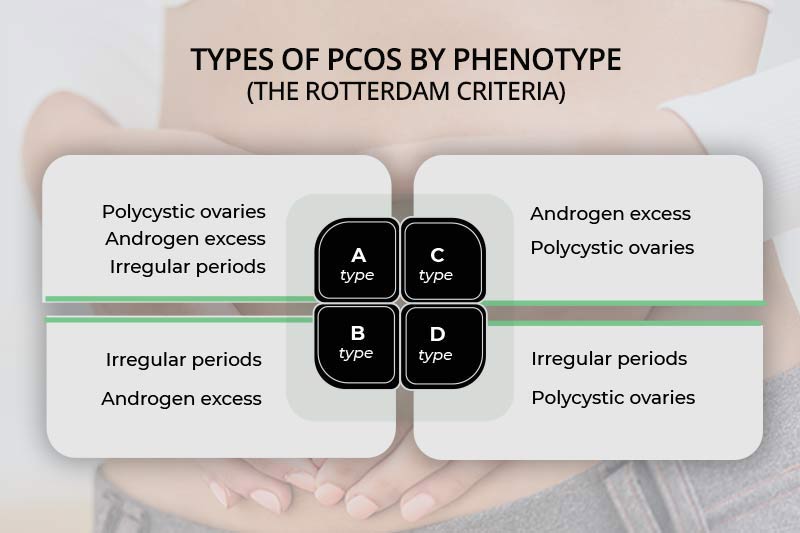
Medical professionals and researchers use the Rotterdam criteria established in 2003 to diagnose polycystic ovary syndrome by the condition’s observable characteristics (phenotype). These criteria state that a person has PCOS when they have two symptoms out of these three:
- Polycystic ovaries – The ovaries are usually larger than typical and covered with many fluid-filled follicles carrying immature eggs.
- Excess androgen (male hormone) – Too much of the male hormone can cause hirsutism (excess body hair), thinning or balding scalp hair, and hormonal acne.
- Irregular or absent periods – Menstrual cycles occur in over a month, don’t occur at all, or last unusually long.
There are four PCOS types by phenotype.
Phenotype A
Patients with phenotype A PCOS, also called classic or full polycystic ovary syndrome, exhibit all three symptoms (excess testosterone, ovulatory dysfunction, and polycystic ovaries).
Phenotype B
Phenotype B or non-PCO PCOS is when the patient has hyperandrogenism and irregular cycles without polycystic ovaries.
Phenotype C
Phenotype C or ovulatory PCOS is when the patient experiences excess male hormone and polycystic ovaries but has regular periods.
Phenotype D
Phenotype D is non-hyperandrogenic PCOS. The patient has polycystic ovaries and irregular periods but normal testosterone levels.
Types of PCOS by Underlying Causes
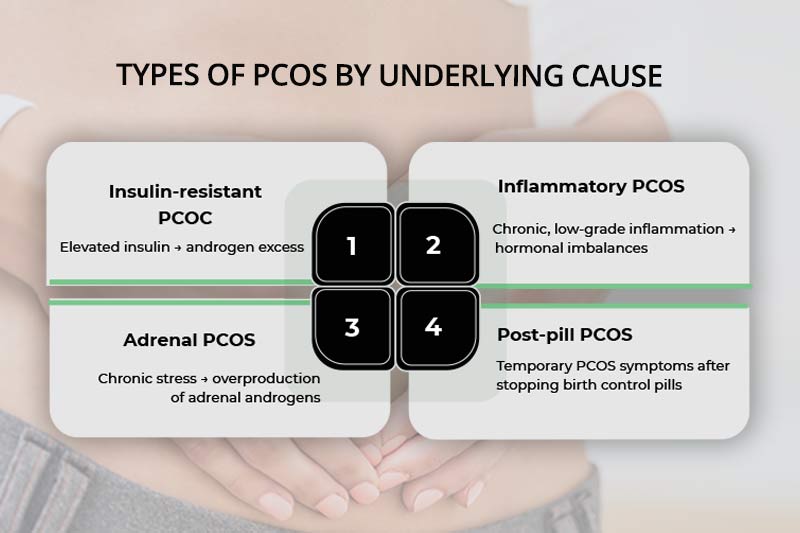
The Rotterdam criteria don’t cover all common accompanying features of PCOS. Hence, a patient’s PCOS type can also be diagnosed based on an underlying cause.
Insulin-Resistant PCOS
Insulin resistance is often associated with polycystic ovary syndrome. Insulin is a hormone that signals the body cells to absorb glucose from the blood and convert it to energy for essential functions. When cells become resistant to insulin and fail to use sugar efficiently, the pancreas compensates by producing more insulin. Elevated insulin levels can stimulate excess androgen production, disrupt hormonal balance, and contribute to the development of PCOS symptoms.
Inflammatory PCOS
PCOS is accompanied by chronic, low-grade inflammation. Long-term inflammation stimulates the ovaries to produce too much testosterone, causing PCOS symptoms. Inflammatory PCOS also leads to digestive problems, joint pain, headaches, and skin conditions (psoriasis, eczema, etc.).
Adrenal PCOS
Chronic stress can increase the production of DHEA-S (dehydroepiandrosterone sulfate), an androgenic hormone produced by the adrenal glands as a precursor to sex hormones. Elevated DHEA-S but normal ovarian androgen levels may indicate adrenal PCOS.
Note: Stress and hormones are related. Lowering cortisol levels leads to hormonal balance.
Post-Pill PCOS
When a patient stops using birth control pills, it can lead to a surge in androgens that temporarily causes typical PCOS symptoms – acne, hirsutism, and irregular periods. This usually occurs 3-6 months after stopping contraception.
PCOS types can overlap, with many patients experiencing a combination of insulin resistance, inflammation, and high DHEA-S levels and suffering from various PCOS symptoms. These overlapping factors make the diagnosis and treatment challenging.
PCOS Causes and Risk Factors
The medical community doesn’t fully understand the exact cause of polycystic ovary syndrome, but they agree it occurs due to a complex interaction between genetic, environmental, and hormonal factors. The following factors increase the risk of developing PCOS.
Genetic Predisposition
Patients with family members who have PCOS have a higher chance of developing the condition. Scientists are still researching potential genes that contribute to PCOS. They have identified several gene variants that may influence insulin signaling, androgen production, and ovarian function.
Insulin Resistance
Insulin resistance leads to more insulin production, which can elevate androgen production and disrupt reproductive function. Excess glucose in the bloodstream also leads to weight gain, exacerbating PCOS symptoms.
Note: Insulin resistance affects weight. Different treatments and lifestyle changes can support your weight loss efforts.
Elevated Androgen Levels
High androgen levels, such as testosterone, can interfere with follicle development, leading to ovarian dysfunction, irregular periods, and infertility. Excess androgens are linked to other hormonal imbalances, including high luteinizing hormone (LH) and insulin resistance.
Gut Dysbiosis
Recent research has found a significant link between PCOS and gut health. Gut dysbiosis (imbalance in the gut microbiota) can lead to inflammation, insulin resistance, and hormonal imbalances, which can result in PCOS.
Being Overweight
Excess weight often drives inflammation and hormonal imbalances, contributing to or exacerbating polycystic ovary syndrome. Most PCOS patients are overweight.
Lifestyle
Poor lifestyle choices, such as high intake of sugary and processed foods, insufficient sleep, chronic stress, and lack of physical activity, can trigger PCOS. Over a longer period, these habits disrupt hormonal activity and cause systemic inflammation, which contributes to PCOS development.
Symptoms of Polycystic Ovary Syndrome

Common symptoms of polycystic ovary syndrome include the following:
- Irregular or missing menstrual periods
- Inability to conceive
- Insulin resistance
- Weight gain
- Hormonal belly fat
- Hirsutism
- Thinning scalp hair
- Hormonal acne
- Brain fog
- Depression
- Anxiety
- Skin tags and dark skin patches
- Skin conditions like psoriasis and eczema
It’s possible to have PCOS without any symptoms or with mild symptoms that patients barely notice until they start trying to get pregnant.
PCOS Diagnosis
Diagnosing polycystic ovary syndrome can be complicated due to overlapping symptoms and symptoms that resemble those of other health conditions.
Most medical providers use the Rotterdam criteria to make a diagnosis. They talk to patients about their symptoms and medical history, and typically perform the following exams:
- Physical examination for signs of excessive hair growth, male-pattern baldness, acne, skin tags, and skin discoloration.
- Blood tests to check for raised reproductive hormone levels - androgens, luteinizing hormone (LH), follicle-stimulating hormone (FSH), progesterone, and estrogen.
- Pelvic exam to establish reproductive organs’ health.
- Ultrasound to check for polycystic ovaries.
Other common tests include:
- Oral glucose tolerance test to determine the presence of insulin resistance.
- Thyroid function tests to rule out hypothyroidism.
- Lipid profile to evaluate cardiovascular risk.
- Prolactin levels to exclude hyperprolactinemia.
- Sleep apnea tests.
After diagnosing PCOS, the medical provider refers the patient to a specialist, such as a gynecologist or endocrinologist, depending on the patient’s PCOS type.
PCOS Health Risks and Complications
Polycystic ovary syndrome increases the risk of certain chronic conditions and health complications.
- Fertility issues - Because PCOS is characterized by polycystic ovaries, a failure to ovulate, and hormonal imbalances, patients have problems conceiving and maintaining pregnancy.
- Type 2 diabetes – Insulin resistance, present in many PCOS patients, is a pre-diabetic condition. Unless the patient reverses the condition with lifestyle habits and medication, it usually leads to type 2 diabetes.
- Cardiovascular diseases – Chronic, low-grade inflammation present in PCOS increases the risk of cardiovascular diseases.
- Metabolic syndrome – High blood pressure, elevated sugar levels, and elevated cholesterol characterize metabolic syndrome. It is associated with an increased risk of heart disease and stroke.
- Non-alcoholic fatty liver disease – Many PCOS patients also have fatty liver disease. The two conditions share the same risk factors, including excess androgens, insulin resistance, and obesity.
- Mental problems – Women with PCOS often experience depression and anxiety due to high testosterone levels.
- Sleep apnea – PCOS increases the risk of sleep apnea, possibly due to high androgens, low estrogen levels, and increased visceral fat.
- Endometrial cancer – An imbalance in progesterone and estrogen levels in PCOS can lead to excessive thickening of the uterine lining (endometrium), increasing the risk of endometrial cancer.
PCOS Treatment
There is no cure for polycystic ovary syndrome. The treatment focuses on symptom management, enabling fertility (if the patient wants to conceive), and preventing health complications.
Health professionals create a customized treatment plan for each patient depending on their symptoms and associated conditions. The treatment plan typically consists of a combination of the following approaches.
1. Weight Loss
Weight loss is the single most helpful strategy an overweight PCOS patient can adopt. Excess weight has detrimental effects on insulin sensitivity, inflammation, sex hormone levels, and overall hormonal activity. Studies show that even a modest weight reduction of 5-10% can significantly improve metabolic and reproductive symptoms in PCOS patients.
A balanced diet, calorie restriction, and regular exercise are vital in weight reduction and management. Patients can also receive professional help from medical weight loss providers.
Note: Learn how PCOS diet can help you relieve the symptoms of this condition.
2. Exercise

Exercise has proven beneficial effects on various health parameters. It relieves stress, improves sleep, increases insulin sensitivity, balances hormones, and may contribute to menstrual cycle regularity. Engage in moderate exercise for at least 150 minutes per week to achieve positive results.
3. Improving Gut Health
Improving gut health can considerably relieve PCOS symptoms by lowering inflammation, balancing hormones, and improving metabolic function. Prebiotic and probiotic supplements and foods rich in these nutrients (fermented foods, fiber-rich fruits and vegetables) promote the proliferation of beneficial gut bacteria, decrease pathogenic bacteria, and support microbiome homeostasis.
4. Medications
Doctors prescribe medications to PCOS patients depending on their condition’s underlying causes. Common pharmaceuticals for the treatment of polycystic ovary syndrome include the following:
- Drugs for stabilizing menstrual regularity, such as estrogen-progestin or progestin-only contraceptives.
- Insulin-sensitizing drugs like metformin.
- Anti-androgens, which inhibit androgen production (e.g., finasteride).
- Gonadotropins, which stimulate the adrenal glands to produce LH and FSH (for women who want to conceive).
- Gonadotropin-releasing hormone agonists, which block the production of LH and FSH (for women who are not trying to get pregnant).
- Lipid-lowering medications like atorvastatin.
- Acne medications, such as oral isotretinoin and topical retinoids.
5. Hair Removal Treatments
Birth control pills and anti-androgens often help with symptoms of hyperandrogenism, such as hirsutism. However, if they don’t work or if the patient is trying to conceive, hair removal treatments are a viable option. Procedures that usually provide longer-lasting results than shaving include waxing, laser hair removal, and electrolysis.
Conclusion
Polycystic ovary syndrome is a common endocrine disorder affecting millions of women in their reproductive years. The symptoms range from mild to severe. Though PCOS can’t be cured, treatments effectively manage symptoms, maximize fertility, and help prevent chronic, life-threatening conditions.


